“We control matter because we control the mind. Reality is inside the skull.”
O’Brien, from “1984” by George Orwell, 1949

(Model with sunscreen on her face, smiling, pointing witih her index finger in a purportedly-secret Masonic “gesture of recognition”.)
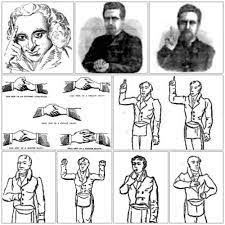
(19th Century depiction of purportedly-secret Masonic “gestures of recognition”, which include the pointing finger being utilized by the model depicting a happy sunscreen user in the photo immediately above.)
I have revised the data section of my sunscreen article, which is pinned here on the U.K. orgones forum.
THE DATA
Sunlight is protective and palliative
The lag time on melanoma is as low as two years. Beaches in the United States were jammed on summer weekends in the 1930s. Why didn’t a melanoma epidemic hit the Depression generation 20 years later? Why did it take until the mid-1970s for the skin cancer epidemic to strike?
From 1981 to 2011, visitors to Cape Cod, Massachusetts decreased by 11%, from 4,978,838 to 4,454,771.
From 1981 to 2011, adjusted for population growth, U.S. visitors to National parks decreased by 10%.
From 1981 to 2011, melanoma cases in the United States increased by an annual average of 5.8%.
From 1981 to 2011, visitors to Cape Cod, Massachusetts decreased by an annual average of .4%.
From 1981 to 2011, U.S. visitors to National parks decreased by an annual average of .33%.
From 1981 to 2011, a .4% decrease in visitors to Cape Cod, Massachusetts was associated with a 5.8% average annual increase in melanoma cases in the United States.
If sun exposure is decreasing, and melanoma is increasing, then sun exposure is protective against melanoma.
From 1981 to 2011, a .33% decrease in visitors to National Parks in the United States was associated with a 5.8% average annual increase in melanoma cases there.
If sun exposure is decreasing, and melanoma is increasing, then sun exposure is protective against melanoma.
From 1998 to 2011, vistors to Cape Hatteras beach park in North Carolina decreased by 28%, from 2,737,640 to 1,969,711.
From 1998 to 2011, visitors to Cape Hatteras beach park in North Carolina decreased by an annual average of 2.2%.
From 1998 to 2011, a 2.2% average annual decrease in visitors to Cape Hatteras beach park in North Carolina was associated with a 5.8% average annual increase in melanoma cases in the United States.
Decreasing sun exposure, increasing melanoma.
The sun is protective against melanoma.
In 2014, women in Sweden who avoided lying out in the sun had mortality twice that of those who sunbathed daily.
Sunlight is protective, palliative.
Sunscreen is not protective against skin cancer
There is no evidence that sunscreen offers any real protection against malignant melanoma, the most dangerous form of skin cancer.
Dermatologists get much of their information from the Skin Cancer Foundation.
The Skin Cancer Foundation is heavily supported by the sunscreen industry. A sunscreen manufacturer funds the Skin Cancer Foundations’s quarterly consumer publication, “Sun and Skin News".
In 1998, Epidemiologist Marianne Berwick of the Memorial Sloan-Kettering Cancer Center in New York, said that “It’s not safe to rely on sunscreen.”
Researchers at the Brookhaven National Laboratory in Upton, New York concluded: “Sunscreens effective in the UV-B region…would not protect against melanoma.”
Suncreens can’t and don’t prevent melanoma, in that most sunscreens do not offer protection against UV-A, the harmful, longer-wavelength UV light that penetrates right through the outer skin—and through sunscreen—down to the melanocytes, the cells that become cancerous in melanoma cases.
If you just use a sunscreen that just protects against sunburn, you are effectively getting the same sun exposure as you would from a tanning bed.
Only avobenzone, is “clearly proven” to block UV-A sunlight. The FDA does not require its inclusion in sunscreens in order for manufacturers to claim that their products offer broad-spectrum protection.
U.S. consumers don’t have access to eight advanced European sun-filtering molecules because the Food & Drug Administration is not convinced they are safe for users. In May 2015, after more than ten years, the FDA would still not allow new sunscreens.
Sunscreen causes skin cancer and breast cancer
The sunscreen ingredients avobenzone, oxybenzone, octocrylene, and ecamsule are absorbed from the skin into the bloodstream after a single day of sunscreen use.
After initial absorption, the concentration of these chemicals in the blood increases each day of application, and remain above FDA safety levels at day seven. Homosalate and oxybenzone remain above safety thresholds at day 21.
Oxybenzone, a known carcinogen, is absorbed into the body at a rate 50 to 100 times greater than any other sunscreen ingredient, where it acts as a photosensitizer and increases the release of free radicals.
In 2008, a study by the US Centers for Disease Control and Prevention found oxybenzone in 97% of urine samples. A 2008 Swiss study found oxybenzone or one of four other sunscreen chemicals in 85% of breast milk samples,
Oxybenzone couples with another common sunscreen ingredient, Retinyl palmitate, which speeds the development of skin tumors and lesions when applied to the skin in the presence of sunlight.
Tumors and lesion development was 21% greater in lab animals coated in a sunscreen containing Retinyl palmitate than in controls.
UV stabilizers in sunscreen products have estrogenicity in an MCF-7 breast cancer cell assay as well as an immature rat uterotrophic assay.
Oxybenzone drives lower testosterone levels in adolescent boys, hormone changes in men, and shorter pregnancies and disrupted birth weights in babies.
Oxybenzone also drives contact allergies. A 10-year study found that 70% of people had a positive patch test when exposed to oxybenzone.
Women 49 or younger have a higher probability of developing melanoma than any other cancer, except breast cancer (which is also driven by sunscreen), or thyroid cancer.
Until around 1950, melanoma was rare. Then its incidence increased slowly until the mid-1960s, when it accelerated into the current epidemic.
From 1972 to 2012, international sunscreen sales increased by 3,510%, from $19 million to $686 million.
From 1972 to 2012, international sunscreen sales increased by an annual average of 87.8%.
From 1972 to 2012, an 87.8% average annual increase in international sunscreen sales was associated with a 4.6% average annual increase in melanoma risk in the United States.
From 1972 to 1996, international sunscreen sales increased by 2,531%, from $19 million to $500 million.
From 1972 to 1996, international sunscreen sales increased by an annual average of 106%.
From 1972 to 1996, a 106% average annual increase in international sunscreen sales was associated with a 4.6% average annual increase in melanoma risk in the United States.
From 1972 to 1996, every 1% increase in international sunscreen sales was associated with a 4.3% increase in melanoma cases in the United States.
If sunscreen sales are increasing, and melanoma risk is increasing, then sunscreen drives melanoma.
From 1980 to 2024, melanoma risk in the United States increased by 200%, or tripled, from 1 in 250, or .4% to 1 in 84, or 1.2%.
From 1980 to 2024, melanoma risk in the United States increased by an annual average of 4.6%.
In 1980, an American’s lifetime melanoma risk was 1 in 250, or .4%.
From 1981 to 2011, the 6.6% average annual increase in sunscreen-driven melanoma cases in the United States was 53.5% greater than their 4.3% average annual increase from 1972 to 1980.
From 1981 to 2011, melanoma cases in the United States increased by 173%, from 26,000 to 71,000.
From 1981 to 2011, an 87.8% average annual increase in international sunscreen sales was associated with a 5.8% average annual increase in melanoma cases in the United States.
From 1981 to 2011, every 1% average annual increase in international sunscreen sales was associated with a 6.6% average annual increase in melanoma cases in the United States
If sunscreen sales are increasing, and melanoma cases are increasing, then sunscreen drives melanoma.
From 1982 to 2015, white women in the younger age groups in the United States, Canada, Australia, New Zealand, the UK, Sweden, Norway, and Denmark have a greater incidence of melanoma than men.
Excess melanomas were found in women younger than 45 years in all populations (eg, IRR for 20-24 y age group, 0.3 in Denmark and 0.7 in Australia).
From 1982 to 2014, melanoma cases in the United States increased by 192%, or nearly tripled, from 26,000 to 76,000.
From 1982 to 2014, melanoma cases in the United States increased by an annual average of 6%.
From 1982 to 1996, a 106% average annual increase in international sunscreen sales was associated with a 6% average annual increase in melanoma in the United States.
If sunscreen sales are increasing, and melanoma is increasing, then sunscreen drives melanoma.
From 1996 to 2012, international sunscreen sales increased by 37%, from $500 million to $686 million.
From 1996 to 2012, international sunscreen sales increased by an annual average of 2.3%.
From 1996 to 2012, a 2.3% average annual increase in international sunscreen sales was associated with a 6% average annual increase in melanoma in the United States.
If sunscreen sales are increasing, and melanoma rates are increasing, then sunscreen drives melanoma.
From 1983 to 2014, the 6% average annual increase melanoma cases in the United States was 30.4% greater than the 4.6% average annual increase in melanoma risk in the United States from 1980 to 1982.
Melanoma cases in the United States are increasing exponentially, going forward in time. What is the variable? Sunscreen use.
From 1982 to 2014, melanoma cases in the United States increased by an annual average of 6%.
In 1999, M. Bigby published “the Sunscreen and Melanoma Controversy” in ArchDermatol, in which he stated “Previous case-control studies have suggested that sunscreen use is associated with an increased risk of melanoma”.
In 2000, P. Autier, M.D. published “Sunscreen and Melanoma Revisited” in ArchDermatol., in which he said "For the last 20 years, epidemiological data have suggested that sunscreen use could increase rather than decrease the risk of cutaneous melanoma.
Epidemiologic data suggest that behavioral issues could be involved in this association between high-factor sunscreen and melanoma."
Where “behavior issues” is general.
As you may recall, generality is a hallmark of propaganda.
From 2006 to 2015, the incidence rate of melanoma in the United States increased by 14.5%, from 200.1 to 229.1 cases per million person-years.
From 2006 to 2015, the incidence of melanoma in the United States increased by an annual average of 1.6%.
From 2012 to 2014, the 6% average annual increase in melanoma rates in the United States was 3.5% greater than its 5.8% average annual increase from 1981 to 2011.
From 2013 to 2023, the number of new invasive melanoma cases diagnosed annually increased by 27 percent.
From 2013 to 2023, the 68.8% positive variance in the average annual increase in melanoma cases in the United States versus 2006 to 2013 was 1,866% greater than the 3.5% positive variance in same from 2012 to 2014 versus 1981 to 2011.
From 2013 to 2023, the 2.7% average annual increase in melanoma cases in the United States was 68.8% greater than their 1.6% average annual increase from 2006 to 2013.
From 2013 to 2023, the 2.7% average annual increase in melanoma cases in the United States was 53.5% less than their 5.8% average annual increase from 1981 to 2011.
In 2015, the 30% of women who regularly used sunscreen was 114% greater, or more than twice as great as the 14% of men who did the same.
In 2024, an American’s lifetime melanoma risk was 1 in 84, or 1.2%.
The populace has recognized the deadly nature of sunscreen.
From 2001 to 2011, the percentage of U.S. teenagers using sunscreen decreased by 12%.
From 2001 to 2011, sunscreen use by teenagers in the United States decreased by an annual average of 1.2%.
From 2001 to 2011, sunscreen use decreased by 17.1%, from 67.7% of study respondents to 56.1%.
From 2001 to 2011, sunscreen use decreased by an annual average of 1.7%.
In 2001, 67.7% of study respondents used sunscreen.
From 2005 to 2016, the 5.4% decrease in melanoma rates among female adolescents in the United States was 22.7% greater than the 4.4% decrease among their male peers.
From 2005 to 2016, melanoma incidence rates among female adolescents in the United States decreased by 5.4%.
From 2005 to 2016, melanoma incidence rates among male adolescents in the United States decreased by 4.4%.
From 2005 to 2016, the 3.7% decrease in melanoma among male young adults in the United States was 2.7% greater than the 3.6% decrease among their female peers.
From 2005 to 2016, melanoma incidence rates among male young adults in the United States decreased by 3.7%.
From 2005 to 2016, melanoma incidence rates among female young adults in the United States decreased by 3.6%.
From 2005 to 2011, the 1.2% average annual decrease in sunscreen use by U.S. teenagers was associated with a 3.7% decrease in melanoma incidence among male young adults and a 3.6% decrease among females.
From 2005 to 2016, melanoma incidence rates among male young adults in the United States decreased by 3.7%.
From 2009 to 2024, Americans who did not used sunscreen increased by 6.5%, from 31% to 33%.
From 2009 to 2024, Americans who did not use sunscreen increased by an annual average of .4%.
In 2009, 31% of Americans did not use sunscreen.
From 2013 to 2023, the 2.7% average annual increase in melanoma cases in the United States was 53.5% less than their 5.8% average annual increase from 1981 to 2011.
In 2014, 32% of study participants never used sunscreen.
In 2014, 14% of study participants always used sunscreen.
From 2015 to 2022, regular sunscreen use in the United States decreased by 13.6%, from 22% to 19%.
From 2015 to 2022, regular sunscreen use in the United States decreased by an annual average of 1.9%.
From 2015 to 2020, the 12.1% decrease in regular sunscreen use by men in the United States was 266.6% greater than the 3.3% decrease among women.
From 2015 to 2020 regular sunscreen use by men in the United States decreased by 12.1%, from 14% to 12.3%.
From 2015 to 2020, regular sunscreen use by women in the United States decreased by 3.3%, from 30% to 29%.
In 2015, 30% of women in the United States regularly used sunscreen.
In 2015, 22% of the populace in the United States regularly used sunscreen.
In 2015, 14% of men in the United States regularly used sunscreen.
In 2020, 12.3% of men and 29.0% of women aged ≥18 years always used sunscreen when outside on a sunny day for >1 hour.
In 2021, 19% of study respondents used sunscreen on a daily basis.
In 2022, 56% of study participants in the United States, rarely or never used sunscreen.
In 2022, 35% of study respondents in the United States did not use sunscreen.
In 2022, 21% of study respondents in the United States wore sunscreen once or twice a year or less.
From 2022 to 2023, the 28.9% decrease in daily sunscreen use in the United States was 1,421% greater than the 1.9% average annual decrease in regular sunscreen use in the United States from 2015 to 2022.
From 2015 to 2022, regular sunscreen use in the United States decreased by an annual average of 1.9%.
From 2022 to 2023, daily sunscreen use in the United States decreased by 28.9%, from 19% to 13.5%.
In 2021, 19% of study respondents used sunscreen on a daily basis.
In 2022, 19% of study respondents in the United States wore sunscreen on a daily basis.
From 2023 to 2024, study participants in the United States who did not wear sunscreen at all increased by 200%, or tripled, from 11% to 33%.
From 2023 to 2024, the 200% increase in Americans who did not use sunscreen was 48,899% greater than their .4% average annual increase from 2009 to 2024.
In 2023, 11% of study participants in the United States did not wear sunscreen at all.
In 2023, 13.5% of study participants wore sunscreen daily.
In 2024, 33% of study respondents did not use sunscreen.
In 2024, the 42% of men who did not use sunscreen were 68% greater than the 25% of women who did not use sunscreen.
In 2024, 25% of women did not use sunscreen.
At this writing in July 2024, Hawaii, the Pacific nation of Palau and Key West have all banned sunscreens containing oxybenzone and octinoxate, because they cause coral bleaching and are dangerous to marine ecosystems.
Jeff Miller, Honolulu, HI, July 9, 2024
If you’d like to be added to this free mailing list, please send me a note at [email protected].